 |
 |
| Encephalitis > Volume 2(3); 2022 > Article |
|
Abstract
Telemedicine is an emerging field of medicine that has become more important during the coronavirus disease 2019 (COVID-19) pandemic era and is being studied actively in various medical fields. In neurology, the introduction of telemedicine is accelerating worldwide under the label of teleneurology. So far, few studies have been conducted on telemedicine for patients with epilepsy. In nonmetropolitan areas, video-based clinics have been demonstrated to be effective for seizure control, and smartphone-based diagnosis has also been confirmed to be accurate. Indeed, after the onset of the COVID-19 pandemic, telemedicine has been used to treat patients with epilepsy around the world. Few studies have examined the use of telemedicine for patients with autoimmune encephalitis. One showed that telephone-based evaluation is sufficient to assess the cognitive reserve of leucine-rich glioma inactivated-1-antibody encephalitis patients, thereby diagnosing their dementia. Telephone-based outpatient clinics are temporarily permitted under Korean medical law, and telemedicine can be attempted for clinically stable patients with epilepsy in Korea. In addition, patients with autoimmune encephalitis in stable or improving status may also be candidates for treatment with telemedicine. This review presents evidence for the safety and efficacy of telemedicine to treat epilepsy and encephalitis patients and discusses indication guidelines. Based on our literature review and current Korean medical law, we suggest tentative guidelines for telemedicine in the fields of epilepsy and autoimmune encephalitis.
The coronavirus disease 2019 (COVID-19) pandemic began in late 2019. As of April 2022, South Korea has experienced 200,000 to 400,000 confirmed cases per day, and 14 million people, a quarter of the population, have histories of COVID-19 infection. New variants of the coronavirus continue to occur, from delta to omicron and stealth omicron, and it is unknown when the pandemic will end. The pandemic has impacted various aspects of the medical environment. In particular, it has exacerbated existing health care disparities [1]. Vulnerable patients have significantly reduced outpatient clinic visits due to the risk of infection and experience related emotional stress [1-3].
In this situation, telemedicine is spotlighted as an alternative to in-person care. Telemedicine is a new method of medical care conducted through telephone, video, or other virtual technologies without visiting patients face-to-face [4]. Telemedicine is being applied not only in internal medicine but also in various other medical fields [5-8]. Recently, it has been tried in neurology, under the label of teleneurology [9,10].
In this review, we outline the study of telemedicine in the field of epilepsy and encephalitis, which are relatively poorly investigated among neurology subfields, and the evidence for the safety and effectiveness of telemedicine compared to in-person visit clinics. In addition, we review Korean medical law and suggest indications for the application of telemedicine in epilepsy and encephalitis treatment based on a literature review. We confirm that we have read the Journal’s position on issues involved in ethical publication and affirm that this report is consistent with those guidelines.
Telemedicine was studied in the epilepsy field before the COVID-19 pandemic era (Table 1). Prior research showed that telemedicine is not inferior for caring for epilepsy patients compared to conventional in-person visits. Between 2009 and 2012, a pilot study among 24 patients with epilepsy was conducted in Arkansas, a nonmetropolitan area in the United States [11]. The authors established a telemedicine epilepsy clinic at the University of Arkansas for Medical Sciences and connected with peripheral sites in the state of Arkansas more than 160 kilometers distant. Two-thirds of the patients in the study had favorable outcomes, with seizure-free or frequency reduction, even patients with refractory epilepsy. In 2017, a prospective randomized study was published comparing the outcomes of epilepsy patients in an Indian single tertiary hospital [12]. For 36 weeks, the authors randomly assigned 465 patients with epilepsy to groups reviewed by telephone and by in-person visits and compared the frequency of breakthrough seizures between them, and found no significant difference between the two groups. Moreover, for the telephone group treatment was more cost-effective and patients were more compliant than the in-person visit group. The accuracy of smartphone-based epilepsy diagnosis was also demonstrated by a prospective multicenter masked clinical trial at eight academic epilepsy centers in the United States [13]. Using only smartphone videos submitted by 44 patients, experts were able to differentiate epileptic seizures from psychogenic or physiologic non-epileptic events with 89.1% accuracy and 93.3% sensitivity.
The COVID-19 pandemic has accelerated research into telemedicine in epilepsy. During the pandemic era, access to in-person visits by patients has been limited around the world, increasing the relative importance of telemedicine. According to the International League Against Epilepsy (ILAE), questionnaires distributed worldwide indicate that the use of telemedicine in epilepsy clinics dramatically increased from 37.8% to 87.3% of respondents during the pandemic [3]. In a Norwegian study, 87% of neurologists answered that they had shifted from in-person visit clinics to telemedicine clinics during the pandemic [14]. Among neurological disorders, telemedicine was particularly satisfactory for the treatment of epilepsy, both for clinicians and patients. Making dosage changes of antiseizure medication (ASM) via telemedicine was effective according to 92% of the clinicians who answered the survey.
It is not surprising that epilepsy was suitable for treatment via telemedicine, given that history taking is the core of medical care for epilepsy patients. More than 90% of clinicians who were involved in a recent study agreed that obtaining a patient history by telemedicine was similar to in-person visits for both new patients (90%) and follow-up patients (98%) [15]. This trend was even stronger in epilepsy because patient consultations are mainly discursive. Several clinicians felt that video-based clinics were sufficient to perform physical examinations of epilepsy patients including mental status, eye movement, shakiness, and unsteady gait.
We hypothesize that telemedicine can be successfully adopted for epilepsy patients in Korea as well. Korea consists mostly of urban areas, and tertiary medical institutions are relatively easy to access compared to other countries. This was one of the objections raised in the debate over whether telemedicine needs to be introduced in Korea. However, studies have shown that telemedicine for epilepsy has high satisfaction in metropolitan as well as nonmetropolitan areas [3,11,15], and the need for remote options is highlighted in the COVID-19 pandemic era. In particular, poor connection or no access to the internet, which is an obstacle to telemedicine, is not a major problem in Korea, which has the highest internet penetration rate of any country in the world.
Encephalitis can be broadly classified into infectious and autoimmune origins according to cause. Infectious encephalitis, including viral and bacterial, generally has a much graver course and most cases require intensive care with poor prognosis. Therefore, this review focuses on telemedicine for autoimmune encephalitis, which requires long-term treatment and outpatient care.
Autoimmune encephalitis was discovered relatively recently [16], with the most prevalent forms being N-methyl-D-aspartate receptor (NMDAR)-antibody encephalitis followed by leucine-rich glioma inactivated-1 (LGI1)-antibody encephalitis [17]. More than 30 types of autoantibodies have been found [17,18], but most autoimmune encephalitis is seronegative [19]. Patients with autoimmune encephalitis are hospitalized for thorough investigations to determine etiology and receive intensive immunotherapy. After primary treatment, patients undergo long-term follow-up care for at least one year, and according to their response to treatment, alternative and boost immunotherapies are often administered. For patients with NMDAR-antibody encephalitis, the follow-up care for full recovery is generally maintained for 12 months [20], and for those with LGI1-antibody encephalitis, many clinicians continue to follow up for 24 months to monitor sequelae regarding the patient's cognition [21,22]. Because of the rarity and specificity of the disease, the evaluation and management for autoimmune encephalitis are performed only at regional base tertiary hospitals or a few specialized tertiary institutions. Therefore, autoimmune encephalitis is an appropriate disease for which telemedicine can be particularly useful, not just during the COVID-19 pandemic era but also in general.
However, compared to its potentiality, telemedicine research in autoimmune encephalitis is limited. Currently, only one study of telemedicine for LGI1-antibody encephalitis has been performed [23]. This study included 37 patients with LGI1-antibody encephalitis who were diagnosed at a single tertiary hospital in Spain and assessed the patients’ cognitive reserve by telephone interview. The questionnaire was composed to measure different aspects of cognitive domains including verbal memory, executive function, and language. Then, the patients’ mood, sleep, and quality of life were also estimated. The authors successfully interviewed 36 patients (97%) and found that 75% of patients had cognitive deficits. The Mini-Mental State Examination and cognitive battery were sufficient to diagnose mild cognitive impairment (MCI) and dementia when administered by telephone. Among the patients, 17% complained of emotional distress and 39% had poor quality of sleep. However, quality of life was not significantly different from healthy controls except for dementia patients. Noticeably, 17 of the 26 patients with good functional status on the modified Rankin Scale (mRS) had MCI. In outpatient clinics, the recovery of patients with autoimmune encephalitis is often evaluated only according to functional status assessed by mRS or Clinical Assessment Scale in Autoimmune Encephalitis (CASE) [24]. This finding suggests that a telephone interview can provide detailed assessments of cognitive reserve, which cannot be clearly identified by impressions in outpatient clinics alone. In summary, telemedicine has the potential to be a sufficient and useful tool for autoimmune encephalitis patients, because monitoring cognitive function sequelae during the long-term follow-up period is important.
Currently, under Article 34 of the Korean Medical Service Act [25], telemedicine is permitted in the form of teleconsults only between medical personnel, defined only as physicians, dentists, or traditional East Asian medical doctors who engage in medical practices. However, since the beginning of 2020, telephone-based clinics have been temporarily allowed due to the COVID-19 pandemic. According to the Ministry of Health and Welfare Announcement No. 2020-177 for the Temporary Allowance of Telephone Counseling or Prescription and Proxy Prescribing [26], telemedicine is intended to prevent members of the public from being infected while visiting medical institutions. Moreover, substitute prescriptions by caregivers have been permitted through telemedicine if the same prescription has been administered for a long period of time while continuing to receive treatment for the same disease. The Announcement limits the use of telemedicine to cases in which safety can be secured according to the physician’s judgment.
If the temporary relaxation of rules allowed during the COVID-19 pandemic era is applied to epilepsy and encephalitis patients, telemedicine is possible for follow-up. In epilepsy, if the ASM has been prescribed for a long time and the patient has had no special side effects, clinicians can care for the patient by telemedicine. Meanwhile, if an encephalitis patient requires follow-up management for symptomatics and functional status evaluation after immunotherapy has been completed, telemedicine is allowed under the current Korean medical law.
However, for telemedicine to be stably implemented in Korea, a number of problems need to be resolved. First, telemedicine is specifically permitted for response to and prevention of the COVID-19 pandemic but is generally prohibited. Even if the law is revised in the future, reimbursement and legal responsibility for medical personnel, which are the decisive reasons that members of the medical community in Korea currently have negative opinions about telemedicine, are the most urgent issues. According to the Announcement, reimbursement and legal responsibility are the same as for in-person clinic visits. However, if telemedicine is implemented broadly, exceptions that were not previously considered will occur, and more case discussions are therefore needed. In addition, in order to implement telemedicine in earnest, unresolved issues including responsibility for the specification of standardized telemedicine devices and management, patient insurance, and protection of privacy should be discussed.
Here in this review, we suggest evidence-based guidelines for the application of telemedicine to the treatment of epilepsy and encephalitis. Permission to use telemedicine in South Korea so far is only temporary. However, there is room for change in Korea’s medical laws on telemedicine, and there is a possibility that telemedicine will be introduced more actively as technology develops.
Telemedicine is recommended for patients with epilepsy in stable condition who have been sufficiently investigated for etiology and do not require additional management other than ASM (Table 2, Figure 1). When a physician prescribes a new ASM to a patient for the first time, in-person visits are favored to titrate the dose and monitor adverse effects. For example, lamotrigine may result in serious skin rash [27,28], but as the patient may not be aware of this side effect it is required to manage the patient face-to-face. In addition, for drugs that may cause dose-related adverse events and oxcarbazepine, which requires hyponatremia measurement [29-32], in-person visits are recommended until dose titration is completed. Telemedicine is applicable for stable patients without breakthrough seizures over a period of ≥3 months. If a breakthrough seizure has occurred but the cause is clear (medication skip, sleep deprivation, emotional stress, etc.), continued management to increase the ASM dose is possible through telemedicine according to physician discretion. However, if the cause is not clear and additional evaluation including an electroencephalogram is required, an in-person visit is strongly recommended.
Telemedicine might be possible in patients who undergo full investigation regarding the etiology of autoimmune encephalitis, and whose condition improves steadily after adequate primary and secondary immunotherapy (Table 2, Figure 2). Encephalitis with known autoantibodies such as NMDAR-antibody encephalitis and LGI1-antibody encephalitis are suitable for treatment via telemedicine due to their relatively well-known prognosis. As noted in the literature review, cognitive function evaluations performed through telemedicine are not significantly different from in-person visits. Therefore, if more frequent evaluation through telemedicine is possible, a better prognosis can be expected. In addition, mRS and CASE, which are function-evaluation items, can be measured by video. If a patient is in stable status without deterioration, remnant seizures and psychiatric symptoms of patients are areas that can be managed with telemedicine according to the physician’s judgment. On the other hand, if aggravation or recurrence is suspected, an in-person visit clinic is recommended for more accurate management and legal liability.
NMDAR-antibody encephalitis is a disease that frequently worsens to mRS 4–5 in the early stage and requires long-term management. For patients with NMDAR-antibody encephalitis, an admission schedule is established according to the immunotherapy plan. Telemedicine can be effective for evaluating the patient's current status and responsiveness to immunotherapy between admissions. If the patient has difficulties with mobility, mRS and CASE can be evaluated more frequently by video, and symptomatic management can be applied through telemedicine for patients whose conditions are stable or improving.
LGI1-antibody encephalitis is a disease in which patients complete immunotherapy in the short term and are followed through outpatient care, so telemedicine is considered to be suitable for treatment. In particular, sequelae such as cognitive dysfunction may remain, so thorough evaluations of cognitive function are required. More frequent evaluation by telemedicine is expected to encourage rehabilitation and alleviate mental stress.
Technological development for telemedicine is already sufficient for broad deployment, and it is therefore being implemented at a very fast rate worldwide. Satisfaction with telemedicine is high for both patients and physicians. Therefore, telemedicine seems to be an unavoidable trend in neurology.
Nevertheless, there are still many problems that need to be overcome for telemedicine to be well established in the treatment of epilepsy and encephalitis. As discussed, the relaxation of regulations for telemedicine in Korea is only temporary, and there is a good chance that it will become banned again after the pandemic is over. In addition, the social discussion is insufficient among those who have an interest in reimbursement, medical insurance issues, and legal responsibility. Since previous research described in our literature review was conducted outside of Korea, further telemedicine studies, including questionnaires tailored for Korean patients, must be conducted in order to introduce telemedicine safely in the Korean medical context. In other words, future studies of the scope and indications for telemedicine should be tailored to the specific circumstances of each country. Our review included evidence for the safety and effectiveness of telemedicine in epilepsy and encephalitis and we have suggested appropriate indications based on this evidence. Therefore, this review can serve as a valuable source for future discussions on telemedicine.
Notes
Figure 1.
Indications for telemedicine in epilepsy
A patient who has a seizure event experiences a stereotypical clinical course. After etiology investigation and antiseizure medication selection, the patient in a stable state visits outpatient clinics regularly unless a breakthrough seizure occurs. According to the evidence and current Korean medical law, telemedicine can replace in-person visits for stable patients in outpatient settings.
OPD, outpatient department; ER, emergency room; EEG, electroencephalogram; VEM, video EEG monitoring.
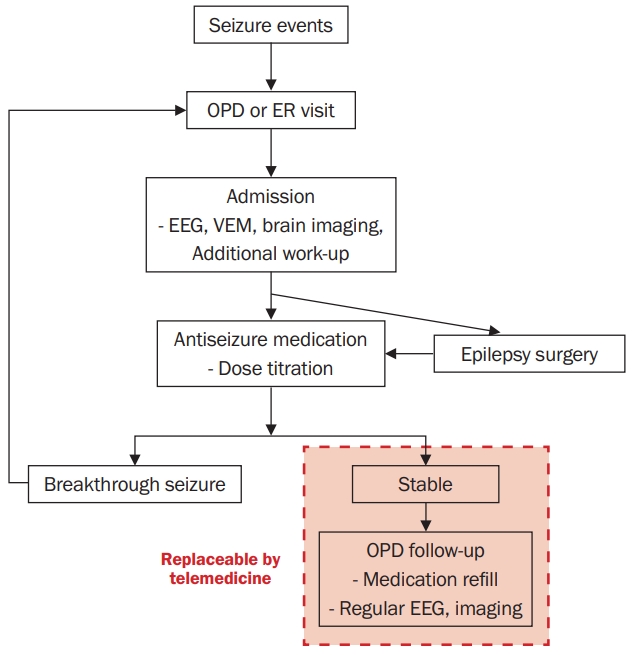
Figure 2.
Indications for telemedicine in encephalitis
A patient who has suspicious symptoms of autoimmune encephalitis undergoes a thorough etiological investigation and receives immunotherapy. After remission, the patient visits outpatient clinics regularly for function evaluation and symptomatic management unless aggravation or recurrence is suspected. In such cases, telemedicine can be recommended for patients in a stable or improving state.
OPD, outpatient department; ER, emergency room; mRS, modified Rankin Scale; CASE, Clinical Assessment Scale in Autoimmune Encephalitis.
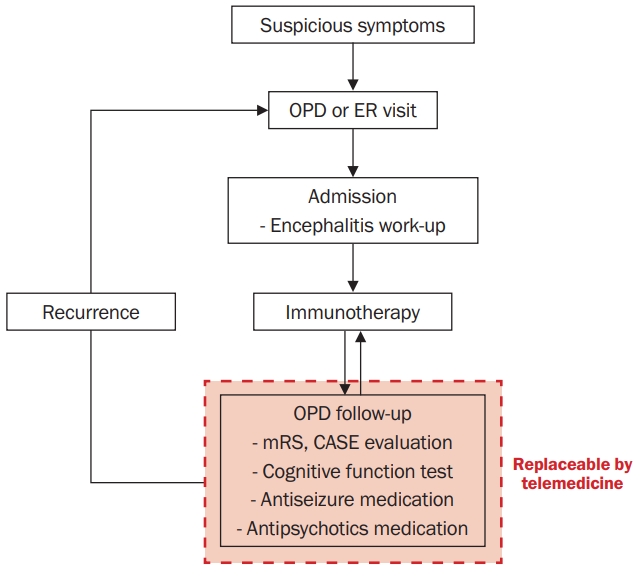
Table 1
Literature review: telemedicine in epilepsy and encephalitis during the COVID-19 pandemic
| Disease | Study | Year | Subject | Center | Length of study (mo) | Evaluation | Results | Conclusion |
|---|---|---|---|---|---|---|---|---|
| Encephalitis | Sola-Valls et al. [23] | 2019 | LGI1-antibody encephalitis patients (n = 37) | Single tertiary hospital in Spain | 87 | t-MMSE, FCSRT, Orall TMT, HADS score, PSQI score, EQ-5D-5L score, mRS | Telephone interviews successful in 97% of patients. Cognitive impairment was detected in 75% of patients. | Telemedicine is comparable to in-person visits for cognitive and functional evaluation in patients with LGI1-encephalitis. |
| Epilepsy | Haddad et al. [11] | 2015 | Epilepsy patients (n = 24) | Single tertiary hospital in the United States | 36 | Seizure outcomes (seizure-free, reduction, unchanged) | Two-thirds of the patients (14/24) had favorable outcomes (seizure-free or 50% reduction of seizure). | Telemedicine can provide effective care for epilepsy patients living in rural areas. |
| Bahrani et al. [12] | 2017 | Epilepsy patients/caregivers (n = 465) | Single tertiary hospital in India | 9 | Number of breakthrough seizures, cost, patient satisfaction with the clinic | There were no significant differences in breakthrough seizures and satisfaction with clinics between the telemedicine group and the in-person visit group. The costs were greater in the in-person visit group. | Telemedicine was not different in terms of breakthrough seizures or patient satisfaction with the clinic compared to in-person visits. | |
| Tatum et al. [13] | 2020 | Epilepsy patients (n = 44) | Eight epilepsy centers in the United States | 36 | Accuracy of smartphone video-based epilepsy diagnosis | Experts diagnosed epilepsy with 89.1% accuracy and 93.3% sensitivity. | Outpatient smartphone video has predictive and additive value for diagnosing epileptic seizures. | |
| Kristoffersen et al. [14] | 2020 | Clinicians (n = 135) | Questionnaire conducted in 17 Norway hospitals | 1 | Proportion switched to telemedicine, satisfaction with telemedicine | In Norway, 87% of neurologists switched to telemedicine for clinic visits. More than 90% of the clinicians were satisfied with telemedicine in epilepsy and had no difficulty in making dosage changes of ASM. | Telemedicine was satisfactory for clinicians, especially in caring for returning patients. | |
| Cross et al. [3] | 2021 | Epilepsy patients/caregivers (n = 590) and clinicians (n = 267) | ILAE website questionnaire conducted worldwide | 5 | Need for telemedicine, barriers against telemedicine | In all, 34.5% of patients/caregivers wished to receive telemedicine care, while 92.1% of clinicians considered telemedicine to be a useful tool. Only 39% of clinicians had difficulties in telemedicine due to poor connections, no access to the new technology by patients, and too many calls. | Telemedicine could be beneficial for epilepsy clinics if adequate infrastructure is present. | |
| Kling et al. [15] | 2021 | Patients/caregivers (n = 25) and clinicians (n = 65) including epilepsy clinic (n = 5 patients, 10 clinicians) | Single tertiary hospital in the United States | 2 | Video adoption, Quality of care, patient-clinician rapport, visit length, history taking, physical exam | Telemedicine was favored for caring for follow-up patients compared to new patients. More than 90% of the clinicians perceived no difference in history taking between telemedicine and in-person visits. | Telemedicine might have utility for epilepsy patients, as the clinic visits are focused on obtaining patient history. |
COVID-19, coronavirus disease 2019; LGI-1, leucine-rich glioma inactivated-1; t-MMSE, telephone Mini-Mental State Examination; FCSRT, Free and Cued Selective Reminding Test; TMT, Trail Making Test; HADS, Hospital Anxiety and Depression Scale; PSQI, Pittsburgh Sleep Quality Index; EQ-5D-5L, 5-level EQ-5D; mRS, modified Rankin Scale; ASM, antiseizure medication; ILAE, International League Against Epilepsy.
Table 2
Indications for telemedicine in epilepsy and encephalitis
References
1. Lopez L 3rd, Hart LH 3rd, Katz MH. Racial and ethnic health disparities related to COVID-19. JAMA 2021;325:719–720.


2. Rosengard JL, Donato J, Ferastraoaru V, et al. Seizure control, stress, and access to care during the COVID-19 pandemic in New York City: the patient perspective. Epilepsia 2021;62:41–50.




3. Cross JH, Kwon CS, Asadi-Pooya AA, et al. Epilepsy care during the COVID-19 pandemic. Epilepsia 2021;62:2322–2332.




5. Tilden DR, Datye KA, Moore DJ, French B, Jaser SS. The rapid transition to telemedicine and its effect on access to care for patients with type 1 diabetes during the COVID-19 pandemic. Diabetes Care 2021;44:1447–1450.




6. Predmore ZS, Roth E, Breslau J, Fischer SH, Uscher-Pines L. Assessment of patient preferences for telehealth in post-COVID-19 pandemic health care. JAMA Netw Open 2021;4:e2136405.



7. Cramer SC, Dodakian L, Le V, et al. Efficacy of home-based telerehabilitation vs in-clinic therapy for adults after stroke: a randomized clinical trial. JAMA Neurol 2019;76:1079–1087.



8. Bellsmith KN, Gale MJ, Yang S, et al. Validation of home visual acuity tests for telehealth in the COVID-19 era. JAMA Ophthalmol 2022;140:465–471.



9. Dorsey ER, Glidden AM, Holloway MR, Birbeck GL, Schwamm LH. Teleneurology and mobile technologies: the future of neurological care. Nat Rev Neurol 2018;14:285–297.



11. Haddad N, Grant I, Eswaran H. Telemedicine for patients with epilepsy: a pilot experience. Epilepsy Behav 2015;44:1–4.


12. Bahrani K, Singh MB, Bhatia R, et al. Telephonic review for outpatients with epilepsy: a prospective randomized, parallel group study. Seizure 2017;53:55–61.


13. Tatum WO, Hirsch LJ, Gelfand MA, et al. Assessment of the predictive value of outpatient smartphone videos for diagnosis of epileptic seizures. JAMA Neurol 2020;77:593–600.



14. Kristoffersen ES, Sandset EC, Winsvold BS, Faiz KW, Storstein AM. Experiences of telemedicine in neurological out-patient clinics during the COVID-19 pandemic. Ann Clin Transl Neurol 2021;8:440–447.




15. Kling SM, Falco-Walter JJ, Saliba-Gustafsson EA, et al. Patient and clinician perspectives of new and return ambulatory teleneurology visits. Neurol Clin Pract 2021;11:472–483.



16. Dalmau J, Gleichman AJ, Hughes EG, et al. Anti-NMDA-receptor encephalitis: case series and analysis of the effects of antibodies. Lancet Neurol 2008;7:1091–1098.



18. Abboud H, Probasco JC, Irani S, et al. Autoimmune encephalitis: proposed best practice recommendations for diagnosis and acute management. J Neurol Neurosurg Psychiatry 2021;92:757–768.



19. Graus F, Titulaer MJ, Balu R, et al. A clinical approach to diagnosis of autoimmune encephalitis. Lancet Neurol 2016;15:391–404.



20. Lee WJ, Lee ST, Shin YW, et al. Teratoma removal, steroid, IVIG, rituximab and tocilizumab (T-SIRT) in anti-NMDAR encephalitis. Neurotherapeutics 2021;18:474–487.




21. van Sonderen A, Thijs RD, Coenders EC, et al. Anti-LGI1 encephalitis: clinical syndrome and long-term follow-up. Neurology 2016;87:1449–1456.


22. Rodriguez A, Klein CJ, Sechi E, et al. LGI1 antibody encephalitis: acute treatment comparisons and outcome. J Neurol Neurosurg Psychiatry 2022;93:309–315.



23. Sola-Valls N, Ariño H, Escudero D, et al. Telemedicine assessment of long-term cognitive and functional status in anti-leucine-rich, glioma-inactivated 1 encephalitis. Neurol Neuroimmunol Neuroinflamm 2019;7:e652.



24. Lim JA, Lee ST, Moon J, et al. Development of the clinical assessment scale in autoimmune encephalitis. Ann Neurol 2019;85:352–358.



25. Korea Ministry of Health and Welfare. Medical Service Act [Internet]. Sejong: Legislation Research Institute; 2020 [updated 2020; cited 2022 Apr 12]. Available from: https://elaw.klri.re.kr/kor_service/lawView.do?hseq=53532&lang=ENG.
26. Korea Ministry of Health and Welfare (MOHW). The temporary allowance of telephone counseling or prescription and proxy prescribing [Internet]. Sejong: MOHW; 2020 [updated 2020; cited 2022 Apr 12]. Available from: http://www.mohw.go.kr/react/al/sal0101vw.jsp?PAR_MENU_ID=04&MENU_ID=040102&CONT_SEQ=353269.
27. Moon J, Park HK, Chu K, et al. The HLA-A*2402/Cw*0102 haplotype is associated with lamotrigine-induced maculopapular eruption in the Korean population. Epilepsia 2015;56:e161–e167.


28. Jang Y, Moon J, Kim N, et al. A new rapid titration protocol for lamotrigine that reduces the risk of skin rash. Epilepsia Open 2021;6:394–401.




29. Jang Y, Yoon S, Kim TJ, et al. Population pharmacokinetic model development and its relationship with adverse events of oxcarbazepine in adult patients with epilepsy. Sci Rep 2021;11:6370.




30. Shin YW, Ahn SJ, Moon J, et al. Increased adverse events associated with antiepileptic drugs in anti-leucine-rich glioma-inactivated protein 1 encephalitis. Epilepsia 2018;59 Suppl 2:108–112.



- TOOLS
-
METRICS

-
- 0 Crossref
- 0
- 3,358 View
- 48 Download
- ORCID iDs
-
Sang Kun Lee

https://orcid.org/0000-0003-1908-0699 - Related articles
 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print



