1. Stojanovich L, Marisavljevich D. Stress as a trigger of autoimmune disease. Autoimmun Rev 2008;7:209–213.


6. Zhu Y, Klomparens EA, Guo S, Geng X. Neuroinflammation caused by mental stress: the effect of chronic restraint stress and acute repeated social defeat stress in mice. Neurol Res 2019;41:762–769.


14. Kaiser S, Sachser N. The effects of prenatal social stress on behaviour: mechanisms and function. Neurosci Biobehav Rev 2005;29:283–294.


15. Pace TW, Mletzko TC, Alagbe O, et al. Increased stress-induced inflammatory responses in male patients with major depression and increased early life stress. Am J Psychiatry 2006;163:1630–1633.


16. Targum SD, Nemeroff CB. The effect of early life stress on adult psychiatric disorders. Innov Clin Neurosci 2019;16:35–37.


19. Murgatroyd C. Epigenetic modifications of early-life stress and adult life psychopathology. In: Teixeira AL, Macedo D, Baune BT, editors. Perinatal inflammation and adult psychopathology. Progress in inflammation research, vol 84. Springer: Cham; 2020.
22. Fagundes CP, Way B. Early-life stress and adult inflammation. Curr Dir Psychol Sci 2014;23:277–283.


29. Susman EJ. Psychobiology of persistent antisocial behavior: stress, early vulnerabilities and the attenuation hypothesis. Neurosci Biobehav Rev 2006;30:376–389.


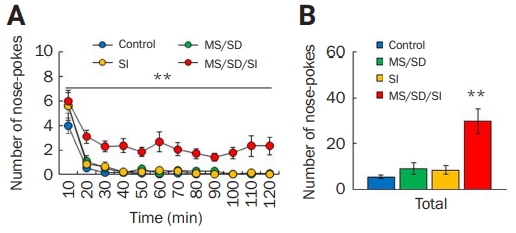
30. Veenema AH. Early life stress, the development of aggression and neuroendocrine and neurobiological correlates: what can we learn from animal models? Front Neuroendocrinol 2009;30:497–518.


31. Gonzalez-Liencres C, Shamay-Tsoory SG, Brüne M. Towards a neuroscience of empathy: ontogeny, phylogeny, brain mechanisms, context and psychopathology. Neurosci Biobehav Rev 2013;37:1537–1548.


32. Lewis CE. Neurochemical mechanisms of chronic antisocial behavior (psychopathy): a literature review. J Nerv Ment Dis 1991;179:720–727.


35. Blair RJ. Neurobiological basis of psychopathy. Br J Psychiatry 2003;182:5–7.


40. Langford DJ, Crager SE, Shehzad Z, et al. Social modulation of pain as evidence for empathy in mice. Science 2006;312:1967–1970.


41. Sachser N, Hennessy MB, Kaiser S. Adaptive modulation of behavioural profiles by social stress during early phases of life and adolescence. Neurosci Biobehav Rev 2011;35:1518–1533.


46. Pryce CR, Dettling A, Spengler M, Spaete C, Feldon J. Evidence for altered monoamine activity and emotional and cognitive disturbance in marmoset monkeys exposed to early life stress. Ann N Y Acad Sci 2004;1032:245–249.


49. Dannlowski U, Kugel H, Grotegerd D, et al. Disadvantage of social sensitivity: interaction of oxytocin receptor genotype and child maltreatment on brain structure. Biol Psychiatry 2016;80:398–405.


50. Lopatina OL, Panina YA, Malinovskaya NA, Salmina AB. Early life stress and brain plasticity: from molecular alterations to aberrant memory and behavior. Rev Neurosci 2020;32:131–142.


52. Radua J, Borgwardt S, Crescini A, et al. Multimodal meta-analysis of structural and functional brain changes in first episode psychosis and the effects of antipsychotic medication. Neurosci Biobehav Rev 2012;36:2325–2333.


55. van Honk J, Schutter DJ. Unmasking feigned sanity: a neurobiological model of emotion processing in primary psychopathy. Cogn Neuropsychiatry 2006;11:285–306.


56. Teicher MH, Ito Y, Glod CA, Andersen SL, Dumont N, Ackerman E. Preliminary evidence for abnormal cortical development in physically and sexually abused children using EEG coherence and MRI. Ann N Y Acad Sci 1997;821:160–175.


58. Hagemann D, Naumann E, Lürken A, Becker G, Maier S, Bartussek D. EEG asymmetry, dispositional mood and personality. Personality and Individual differences. Personal Individ Differ 1999;27:541–568.

59. Decety J. The neural pathways, development and functions of empathy. Curr Opin Behav Sci 2015;3:1–6.

60. Clark AP, Bontemps AP, Batky BD, Watts EK, Salekin RT. Psychopathy and neurodynamic brain functioning: a review of EEG research. Neurosci Biobehav Rev 2019;103:352–373.


62. Anckarsäter H. Central nervous changes in social dysfunction: autism, aggression, and psychopathy. Brain Res Bull 2006;69:259–265.


63. Singer T. The neuronal basis and ontogeny of empathy and mind reading: review of literature and implications for future research. Neurosci Biobehav Rev 2006;30:855–863.


65. Isoda M. The role of the medial prefrontal cortex in moderating neural representations of self and other in primates. Annu Rev Neurosci 2021;44:295–313.


66. Hernandez-Lallement J, van Wingerden M, Kalenscher T. Towards an animal model of callousness. Neurosci Biobehav Rev 2018;91:121–129.


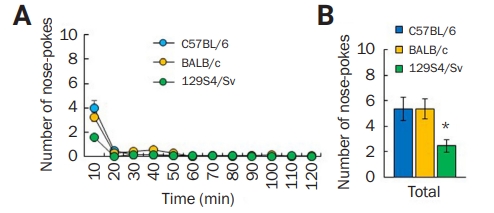
70. Eleftheriou BE, Bailey DW, Denenberg VH. Genetic analysis of fighting behavior in mice. Physiol Behav 1974;13:773–777.


71. Schneider R, Hoffmann HJ, Schicknick H, Moutier R. Genetic analysis of isolation-induced aggression. I. Comparison between closely related inbred mouse strains. Behav Neural Biol 1992;57:198–204.


72. Guillot PV, Chapouthier G. Intermale aggression and dark/light preference in ten inbred mouse strains. Behav Brain Res 1996;77:211–213.







 PDF Links
PDF Links PubReader
PubReader ePub Link
ePub Link Full text via DOI
Full text via DOI Full text via PMC
Full text via PMC Download Citation
Download Citation Print
Print



